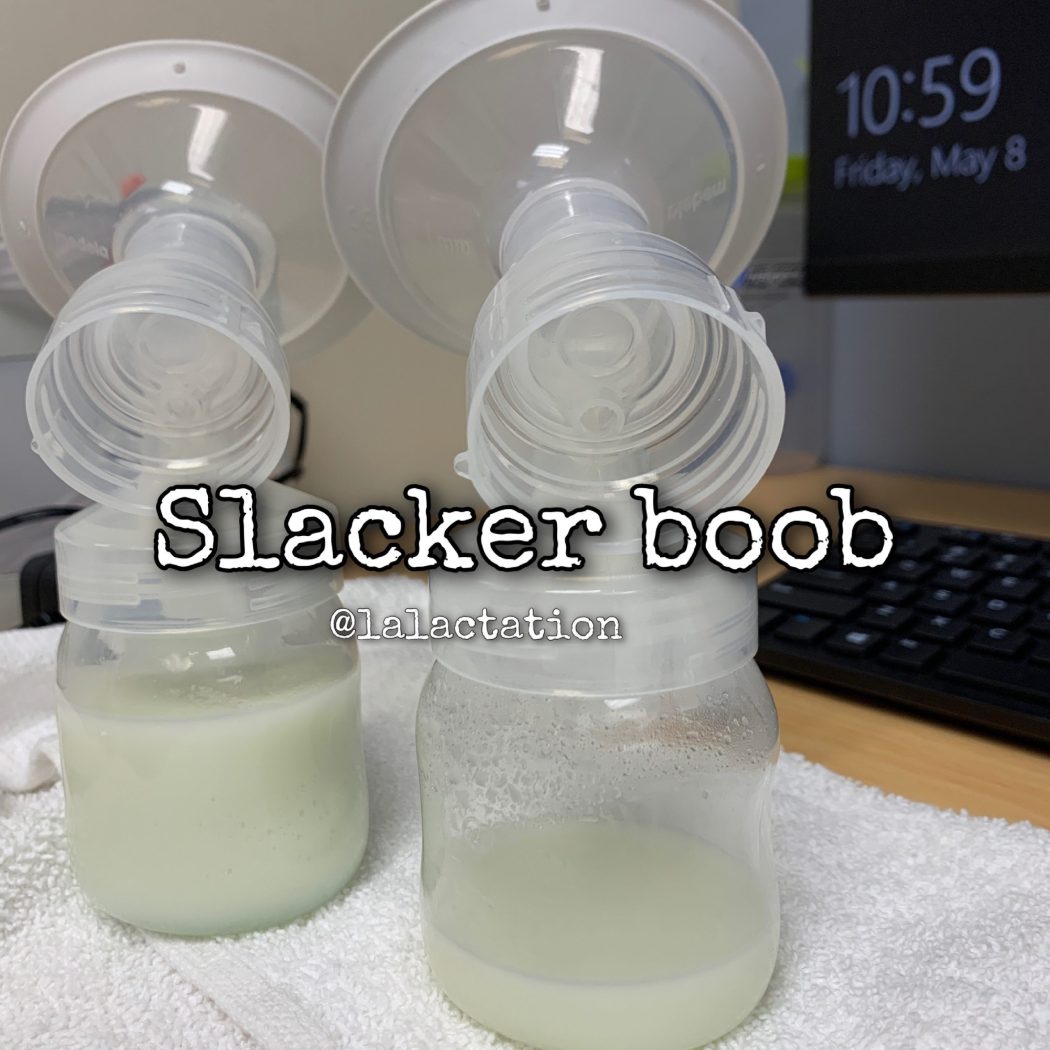
Did you know? Around 70% of women produce more milk in the right breast. Which means 30% make more in the left. It is VERY common for one side to produce more than the other. Some times double on one side. We don’t know why. This is not a reason to neglect one side. You want to make sure you rotate which breast you offer first. Babies may prefer one side over the other for various reasons:
👶🏽They like to lay with their head in a certain direction or their body is uncomfortable in the opposite position
👶🏿They prefer the flow (one side may flow faster or slower than the other)
👶🏼They may prefer the flavor (YES!! Milk can taste different form each breast during the same feeding!!)
If you want to help balance out a slacker boob:
🔆Offer the slacker first more often.
🔆End on the slacker can also help, especially if baby just wants to use you like a pacifier.
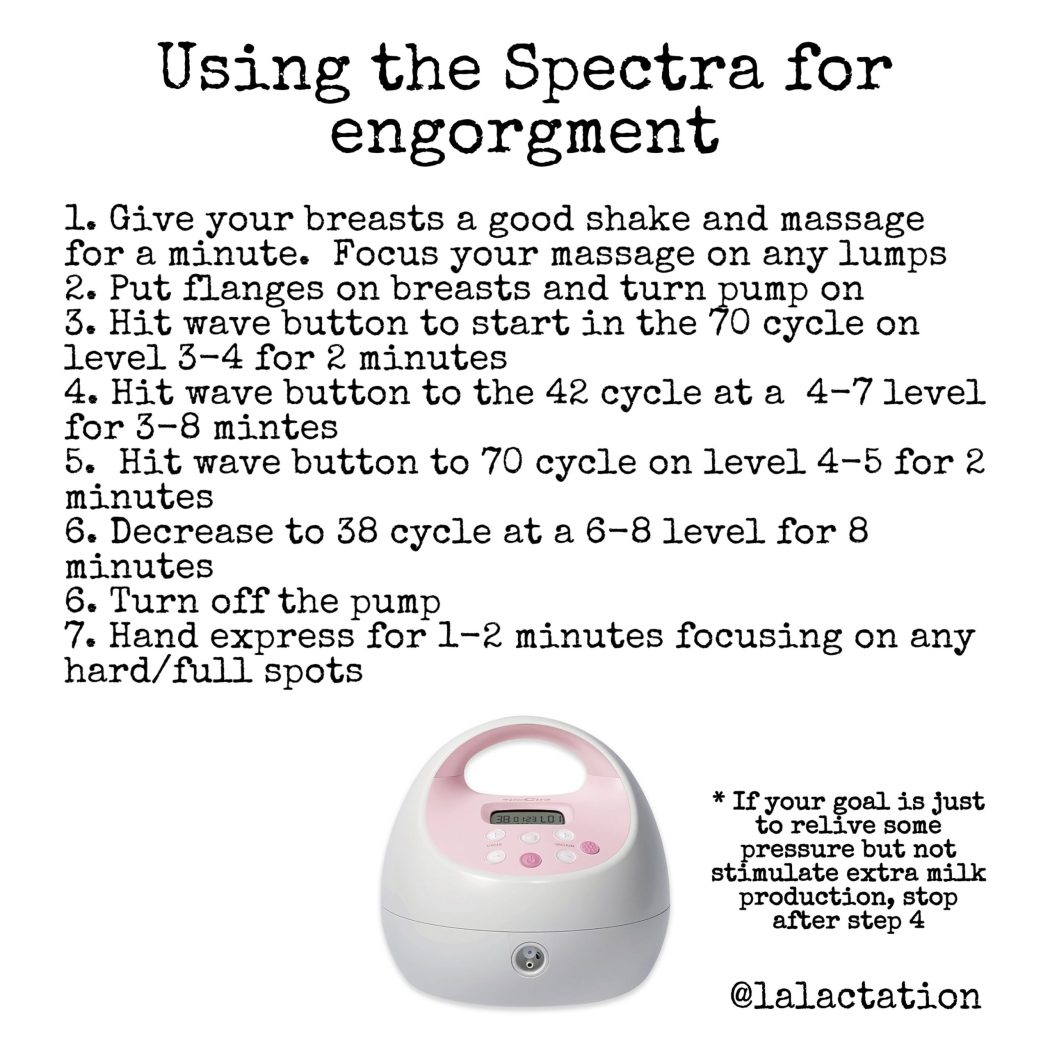
🔆Pump the slacker side during or after feedings can also help stimulate more milk production
🔆Make sure you have the correct sized pump flange on the slacker side. Our nipples can often be different sizes and using the wrong sized flange can drop supply on that side
🔆Hand expression on that side at random times of the day even for a few minutes will jump start increased production.
🔆If it’s positional from your baby (they only want to lay cross cradle to the right and not the left, experiment with other positions like football or side lying to help baby compensate for their body. If your baby prefers one side of the other from a positional perspective, consider taking your baby for some infant bodywork like chiropractic or craniosacral therapy.